Myeloproliferative Neoplasms (MPN)
Myeloproliferative Neoplasms (MPN) are a group of rare blood cancers where the bone marrow makes too many red blood cells, white blood cells, or platelets. This overproduction causes the blood to thicken, increasing the risk of clots, bleeding, and progression to more aggressive blood cancers such as acute myeloid leukaemia (AML).
These disorders are often long-term but manageable with the right treatment and monitoring.
Types of Myeloproliferative Neoplasms
1. Polycythemia Vera (PV)
- Overproduction of red blood cells
- Can cause headaches, dizziness, blood clots
2. Essential Thrombocythemia (ET)
- Excess platelet production
- Increases risk of clotting or bleeding
3. Primary Myelofibrosis (PMF)
- Bone marrow becomes scarred (fibrosis)
- Leads to anemia, weakness, enlarged spleen
4. Chronic Myeloid Leukaemia (CML)
- Characterized by the presence of the Philadelphia chromosome
- Often treatable with targeted therapies (TKIs)
Causes and Risk Factors
MPNs occur when genetic mutations cause uncontrolled growth of blood cells. Risk factors include:
- Mutations in JAK2, CALR, or MPL genes
- Older age (most diagnosed after 50)
- Family history of blood disorders
- Exposure to radiation or toxins (rare)
Symptoms of MPN
Some patients may have no symptoms at first. When present, symptoms can include:
- Headaches, dizziness, or vision problems
- Unexplained itching, especially after a hot shower
- Fatigue and night sweats
- Unexplained weight loss
- Enlarged spleen (abdominal fullness)
- Easy bruising, bleeding, or blood clots
Early detection reduces complications such as stroke or progression to leukaemia.
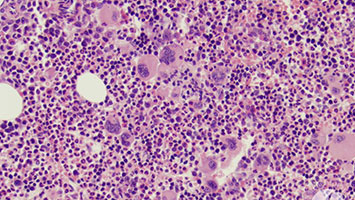
Diagnosis and Tests
MPNs are diagnosed with a combination of blood and genetic tests:
- Complete blood count (CBC) – abnormal levels of blood cells
- Bone marrow biopsy – checks cell growth and fibrosis
- Genetic mutation tests (JAK2, CALR, MPL, BCR-ABL1)
- Ultrasound or imaging to assess spleen size
Treatment Options
Treatment depends on the type of MPN and the patient’s risk level. Options include:
- Phlebotomy (blood removal) for Polycythemia Vera
- Medications: hydroxyurea, ruxolitinib, interferon
- Targeted therapy (TKIs for CML, JAK inhibitors for MF)
- Low-dose aspirin to reduce clotting risk
- Stem cell transplant in severe or high-risk cases
Treatments can help control symptoms, reduce risks, and improve survival.
Living with MPN
Managing MPN requires ongoing monitoring and healthy lifestyle changes:
- Regular follow-up with a hematologist
- Managing cardiovascular risks (blood pressure, cholesterol)
- Staying active and eating a balanced diet
- Emotional support and patient groups
Get Involved
Support makes a difference for patients with MPN:
- Donate blood to help patients needing transfusions
- Spread awareness about early detection
- Participate in clinical trials and research initiatives
Need Support?
- If you or a loved one is affected by MPN, reach out to us at [85 85 85 88 28] for guidance and care.
