Myelodysplastic Syndromes (MDS)
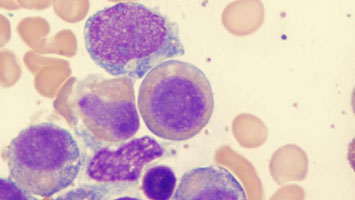
Myelodysplastic syndromes (MDS) are a group of disorders caused by poorly formed or dysfunctional blood cells due to abnormal development in the bone marrow. In MDS, the bone marrow does not produce enough healthy red blood cells, white blood cells, or platelets, leading to anemia, infections, and bleeding problems.
MDS is sometimes referred to as a "bone marrow failure disorder" and in some cases, it can progress to acute myeloid leukaemia (AML).
Types of Myelodysplastic Syndromes
1. Refractory Anemia
- Low red blood cell counts
- Commonly causes fatigue and weakness
2. Refractory Cytopenia with Multilineage Dysplasia (RCMD)
- Multiple blood cell lines affected
- Common in older adults
3. Refractory Anemia with Excess Blasts (RAEB)
- Higher number of immature cells (blasts)
- Greater risk of progression to AML
4. Therapy-Related MDS (t-MDS)
- Develops after prior chemotherapy or radiation
- Often more aggressive
Causes and Risk Factors
MDS can occur without a clear cause, but risk factors include:
- Older age (most patients are over 60)
- Previous chemotherapy or radiation therapy
- Exposure to toxic chemicals (e.g., benzene)
- Genetic mutations or family history
- Smoking
Symptoms of MDS
Symptoms vary but are often related to low blood counts:
- Persistent fatigue and weakness
- Pale skin (anemia)
- Frequent infections (low white cell counts)
- Easy bruising or prolonged bleeding (low platelets)
- Shortness of breath
- Unexplained weight loss
Early detection is important to manage progression and prevent complications.
Diagnosis and Tests
MDS is diagnosed using:
- Complete blood count (CBC) – shows low levels of blood cells
- Bone marrow biopsy – reveals abnormal cell development
- Genetic and molecular tests – detect mutations linked to MDS
- Cytogenetic analysis – checks for chromosomal abnormalities
Treatment Options
Treatment depends on the type of MDS, patient’s age, and overall health. Options include:
- Supportive care (blood transfusions, antibiotics, growth factors)
- Medications (azacitidine, decitabine, lenalidomide)
- Targeted therapy for specific mutations
- Stem cell (bone marrow) transplant – the only potential cure
- Clinical trials for new treatments
While not always curable, treatment can improve quality of life and slow progression.
Living with MDS
Long-term care and support can make a difference:
- Regular monitoring of blood counts
- Nutrition and exercise for strength
- Psychological and social support
- Access to patient support groups
Get Involved
You can help patients with MDS by:
- Donating blood or platelets
- Raising awareness in your community
- Supporting MDS research organizations
- Volunteering for patient assistance programs
Need Support?
- If you or someone you know is affected by MDS, we're here to help. Contact us at [85 85 85 88 28].
